Campylobacter in Poultry: a Worldwide Approach to Diagnosis and Control
US - A synopsis of the 2013 American Association of Avian Pathologists (AAAP) Annual Meeting by Eric Gingerich, DVM, for Diamond V.Six presentations were given on various aspects of diagnosis and control of Campylobacter spp. associated with poultry at this symposium held in conjunction with the recent AAAP Annual Meeting in Chicago.
Background information
Campylobacteriosis in humans is among the most common causes of diarrheal disease worldwide. In the US during 2011, Campylobacter spp. was the 4th leading cause of US foodborne illness at nine per cent of all estimated annual illnesses (845,000) after 1) norovirus (58 per cent), 2) Salmonella spp. (11 per cent), and 3) Cl. perfringens (10 per cent). Since establishment of the baseline in 2008, the prevalence of campylobacteriosis in 2012 has increased 14 per cent from 12.5 per 100,000 to 14.3 per 100,000 persons. Most of the reported outbreaks in humans are due to consumption of undercooked chicken meat. One study using retail meat showed that 95 per cent of the isolates from chicken were C. jejuni.1
Illness caused by Campylobacter spp. was first described by Theodor Escherish in 1886, but successful isolation of the causative organism was not accomplished until 1972.2 Initially classified as vibrios, Sebald and Veron in 1963 proposed the genus Campylobacter as these “slender, curved bacilli”, which differed from the classical cholera and haolphilic vibrios. The term Campylobacter is derived from the Greek words kampylos (curved) and the word baktron (rod) that describes this genus of gram-negative, curved or spiral rods.
Synopses of the presentations (title and presenter) given at the symposium follow.3
Why is it important to control Campylobacter infections?
Robert Tauxe MD MPH, CDC, Atlanta GA, said that the dominant pathogen is C. jejuni in humans and causes an acute gastroenteritis with fever, bloody diarrhea, and painful abdominal cramps. The disease usually resolves in five to seven days but may be more prolonged and systemic in immunocompromised people. About 1 in 1,000 people develop a post-infection paralysis called Guillain-Barre Syndrome. Antibiotics such as fluoroquinolones or azithromycin are used for treatment.
Most infections are foodborne (80 per cent) with the rest being waterborne or resulting from direct contact with animals. The leading risk factor in acquiring campylobacteriosis seems to be consumption of contaminated poultry. Raw milk is also an intermittent source of outbreaks.
Active surveillance through FoodNet, a set of 10 public health departments in various sites throughout the US, has shown a 14 per cent,increase in the frequency of Campylobacter infections since 2006. Prior to that, the frequency had declined 30 per cent from the late 1990s attributed to improvements in poultry processing.
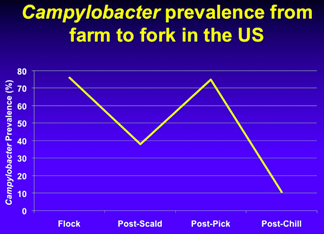
Tracking Campylobacter prevalence and load in the broiler production system
Randy Singer, Department of Veterinary and Biomedical Sciences, University of Minnesota, St. Paul MN, showed a positive correlation for Campylobacter isolation between broiler farms and the processing plant. This leads to the suggestion that downstream effectiveness of on-farm interventions can be predicted with on-farm sampling. In other words, lower counts on boot sock samples at the farm predict a lower incidence and count of Campylobacter on carcasses. The distribution of isolates (1,923) from the study was 84 per cent C. jejuni, 10 per cent C. coli and six per cent both.
WHO Collaborating Center for Campylobacter and OIE Reference Laboratory of Campylobacteriosis
Jaap Wagenaar DVM PhD, Utrecht University, The Netherlands, explained that the European approach for pathogen reduction has been to look at both on-farm and in-plant interventions in order to reduce the level of contamination of poultry meat products. Unfortunately, very effective interventions such as specific chemical washes or irradiation have met with an unacceptable level of consumer resistance. He referenced the Global View Report of a World Health Organization (WHO) meeting on Campylobacter.
What’s old is again new: Difficulty with culturing for Campylobacter
Microbiologists have only been working with Campylobacter spp. pathogens since it was first isolated in 1972, a relatively short time compared to Salmonella which was isolated in 1884, explained Margie Lee DVM PhD, The University of Georgia, Athens GA.
A variety of procedures are used by research and food safety labs to isolate Campylobacter and usually involve an initial enrichment step using nutrient rich broths enhanced with antimicrobials followed by plating on selective agar plates. At this point, little standardisation of procedures exists. It is, therefore, important to use a procedure for your sample of interest that has been previously proven to work.
What is known about Campylobacter control in the processing plant environment?
In his presentation, Scott Russell PhD, The University of Georgia, Athens GA, said that the control of Campylobacter will require different on-farm strategies from Salmonella as the two types of bacteria are adapted to different environments. Campylobacter can reach very high levels of colonization in the chicken ceca, up to a billion organisms per gram. It only takes as few as 40 organisms to infect a bird. Once Campylobacter colonisation starts in a flock, 100 per cent of the flock can be infected within a few days. On-farm methods of control will likely be limited to attempts to decrease levels of infection rather than reducing the within flock prevalence.
The key to reducing Campylobacter will be the use of multiple intervention strategies. It has been shown that a high level of contamination at the start of processing (75 per cent of birds contaminated, EU and US averages) to 11 per cent through the scalding, picking, chemical intervention (online reprocessing system (OLR)), the chiller, and the post-chill dip (finishing chiller). This means that the level of contamination is reduced on 75 per cent of the chickens from the national average of 9,000 colony forming units (CFUs) and as high as one billion CFUs per ml and completely eliminate Campylobacter on 64 per centof the chickens.
Additional chemical interventions are being considered during scalding and post-pick (strong acid mixtures) to further reduce Campylobacter levels especially during summer months when a further 3-log10 reduction may be needed to achieve the 10.4 per cent and below positive standard. In Europe, chemical interventions are not used hence a much higher level of contamination reaches their consumers; 76 per cent of chickens.
Physical interventions such as bird brush systems to reduce faecal contamination on carcasses prior to reaching the scalder will reduce the load entering the scalder.
The level of contamination that comes from the farm will be highly related to how a plant will be able to comply with the present standard of 10.4 per cent or less positive carcasses. A plant receiving chickens with 10 million to one billion CFUs per ml on carcasses may fail this standard since a plant may be able to only achieve a 6- to 8-log10 reduction.
Dr Russell’s suggestion is that the standard should be based on how effective a plant is in reducing numbers on the carcass rather than a percentage of positive carcasses.
How the incidence of human cases of campylobacteriosis in New Zealand was reduced by 50 per cent: Roles played by government, industry and academia
Nigel P. French of Massey University in New Zealand said that the human incidence of Campylobacter increased dramatically from 2000 to 2007 with a peak of approximately 16,000 cases per year. Pressure was placed on the poultry industry to decrease the human illness rate as poultry meat consumption was associated with the illnesses. Today, a level of 8,000 illnesses per year have been recorded, achieving a 50 per cent reduction.
The reduction in human cases was due to the introduction of performance targets for Campylobacter based on enumerated levels on poultry carcasses sampled at the end of the primary processes. If performance targets were not met, escalating regulatory responses were enacted. The plants met the targets through the use of interventions including hygienic practices throughout production and processing (especially immersion chiller conditions). Even with this 50 per cent reduction, New Zealand still has one of the highest rates of human Campylobacter in the world so much work is left to be done.
Summary
Most reductions in Campylobacter on chicken products in the US have been accomplished using control methods in the processing plant. Research is being conducted to investigate if dietary gut health additives can reduce the level of Campylobacter in caecal contents and on birds as they enter the plant. Recent research indicates that Diamond V Original XPC shows promise in reducing this bacterial infection on the farm.
References
- Wong T.L., Hollis L., Cornelius A., Nicol C., Cook R. and Hudson J.A. Prevalence, numbers, and subtypes of Campylobacter jejuni and Campylobacter coli in uncooked retail meat samples. J Food Prot. 70(3):566-73.
- Campylobacteriosis Outbreak. Emerging Infectious Diseases,, 19(8). August 2013.
- Taken from the 2013 AAAP Campylobacter Symposium Abstracts